This document compares prolotherapy and perineural injection treatment (PIT) in a different way, with a few illustrations which may be helpful.
Comparing Prolotherapy and Perineural Injection Treatment (PIT)
Note several images are from Reeves KD, Lyftogt J Prolotherapy: Regenerative Injection Therapy. In: Waldman SD (ed): Pain Management. Philadelphia; Saunders (Elsevier), 2nd ed; 2011:1027-1044. Images from this handout should not be placed on other web sites without permission from Elsevier.
Prolotherapy: Injection with the goal to repair weakened or stretched ligaments or tendons or stabilize joint surfaces affected by arthritis. The term Proli is Latin for “to grow.”
How Does Prolotherapy Work? Dextrose injection (12.5% to 25% concentration) stimulates a brief arachidonic acid (AA) pathway inflammation. AA inflammation is the type of inflammation to which most doctors are referring when they use that word. After an injury, the body uses primarily AA inflammation to try to repair the damage. With prolotherapy there is no significant damage, because there is no stretching or tearing of fibers, but the body still begins a repair process, which allows the structure to become stronger and tighter rather than first becoming weaker and looser.
Why do some people get better quickly with prolotherapy? Healing takes months, but some patients get better quickly. This is likely because dextrose and other solutions have effects on nerves as well. This will be described in the nerve section below.
What about injecting other solutions than dextrose? There are other solutions that stimulate the AA type of inflammation, such as phenol, and they are also called prolotherapy. However, when cells are removed from the human body and then re-injected, that is “biologic repair injection.” The primary goal is still repair but it is by use of tissue from living (biologic) sources. This includes injection of whole blood, stem cell injection and platelet rich plasma injection.
Perineural Injection Therapy (PIT): Injection close to nerves with a goal to restore normal function in nerves that cause chronic pain and degeneration.
How PIT Works: There is another type of inflammation that has been recognized, and that is called neurogenic inflammation. This type of inflammation is produced by special small sensory nerves that are protein producing (“peptidergic”). These nerves normally produce proteins that can be healing or damaging. Neurogenic inflammation occurs when a nerve produces painful or damaging proteins. There are many scientific articles published each month on this type of inflammation.
1. Direct reduction of neurogenic inflammation by dextrose: Dextrose injection in low concentration (5%) reduces neurogenic inflammation. This does not stimulate AA inflammation; the primary intent is to treat nerves, not ligaments, tendons, or cartilage. The primary intent is not to grow new tissue.
2. Loosing areas of constriction about nerves: Using ultrasound, nerves can be located and separated from layers of tissue that tend to compress them and interfere with function. Under ultrasound guidance, injection of dextrose containing fluid can be injected to pull the nerve free from its constriction and the dextrose can then more effectively help the nerve function normally.
“Bad Nerves”, Nerve-Based Inflammation, and Why Arthritis Meds Don’t Help
The “Dr. Jekyll and Mr. Hyde” of chronic pain - TRPV-1 Nerves.
In the story of Dr. Jekyll and Mr. Hyde, Dr. Jekyll drinks a potion that causes him to switch back and forth between a very good Dr. Jekyll and a very evil Mr. Hyde. In 1997, a very important protein structure was completely identified to the point it was successfully reproduced (cloned). This protein structure sits on the surface of all protein-producing (peptidergic) nerve cells, and functions as a channel for ions because positive ions move through it as it opens and cannot move through it when it is closed. If the ion channel is “mellow” (down-regulated), the nerve cell will be very “good” (produce healthy, non-pain producing proteins). If the channel is “over-active” (up-regulated), then the nerve cell will be very “evil/bad” (produce damaging and pain-producing proteins). Thus, this small protein channel on the surface of the nerve cell is the “potion” that will make the nerve cell quickly (in seconds) change its character from “very good” to “very bad.” This ion channel is called the TRPV-1 (transient receptor potential vanilloid - Type 1) channel. We will call the sensory nerves that are controlled by this channel “TRPV-1 nerves.” TRPV-1 sensory nerves supply virtually all areas and is termed the “peptidergic sensory system” because of the ability of these nerves to make proteins (peptides) to affect other structures.
Why Anti-Inflammatory Medications Don’t Work for Neurogenic Inflammation.
Anti-inflammatory medications target AA-inflammation and often do so by blocking cyclooxygenase. Blocking cyclooxygenase does not affect the neurogenic inflammation pathways. Anti-inflammatory medications have some pain-relieving ability other than just by blocking AA inflammation, so they can be useful, although seldom strikingly useful.
Why hasn’t a pill been developed that can treat neurogenic inflammation? There are no safe oral medications (so far) to treat neurogenic inflammation, because they cause high body temperature in clinical trials. Since TRPV-1 nerves supply so many areas, blocking them all with a drug causes unfavorable changes.
How Do Bad Nerves Affect Other Structures; i.e., ligaments, tendons, and cartilage) and Cause Chronic Pain?
Hilton’s Law: TRPV1 nerves connect to all other structures and interconnect with each other.
Hilton’s Law indicates that nerves that cover the skin are joined by nerves from joints, ligaments, and tendons on their way to the spinal cord.
“Switching Road Signs”
- How to transport good or bad proteins to ligaments, tendons, joints, and nerves.
How to Make A TRPV-1 Nerve Behave Badly, and Why Nerves Under the Skin Are Commonly Affected
|
“Claustrophobia”
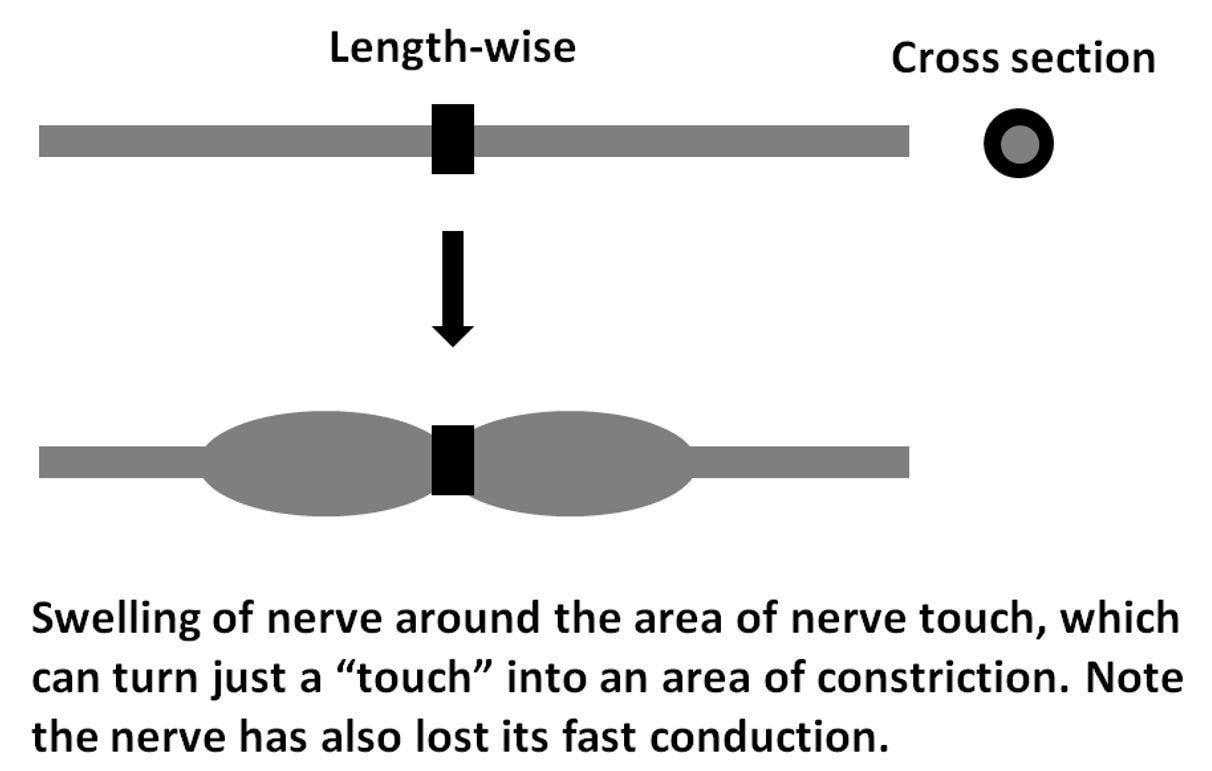
An important quality of TRPV-1 sensory nerves. Animal studies have clearly demonstrated that simply surrounding a nerve around its entire circumference, even without squeezing it, will shut off fast conduction in that nerve, and cause it to behave abnormally. This depiction illustrates how merely touching a nerve on all sides will lead to a swelling reaction. Although the nerve was merely touched, the area can become a point of constriction as the nerve swells on either side of the constriction. Those patients that have heard of Morton’s Neuroma in feet may be interested that this is how nerves in the feet swell up and become neuromas. |
“Skin Nerves” in humans are very easy to damage and become pain sources
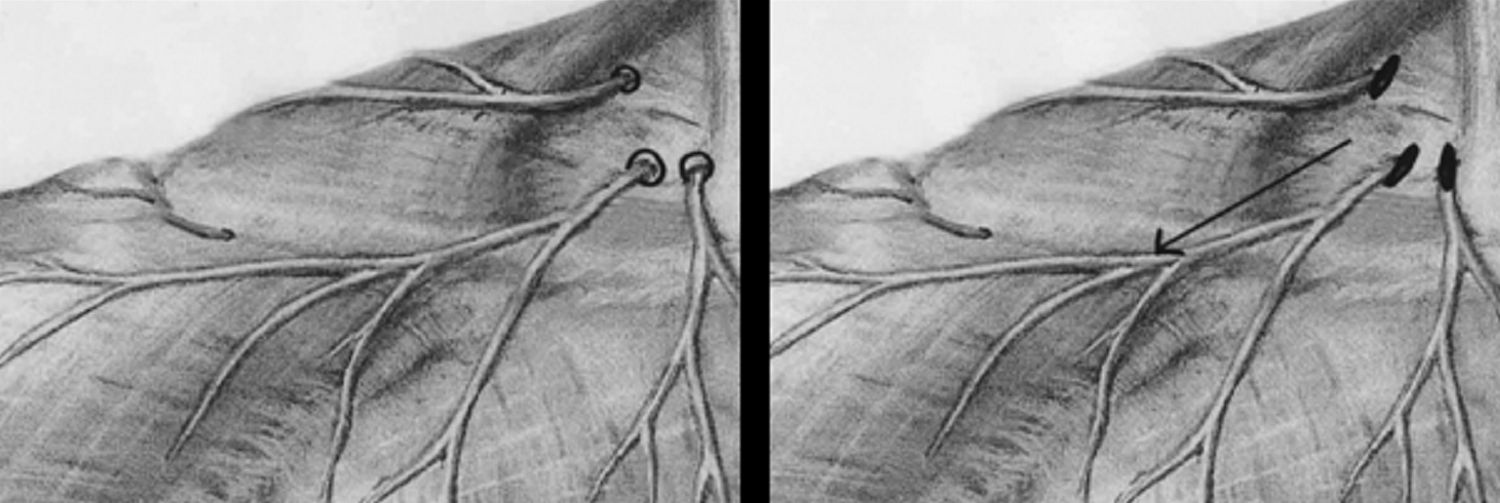
The figure to the left below shows how sensory nerves travel along the skin and then suddenly dive through a layer of fascia to make their way between muscles to travel deeper toward the spinal cord. The first figure shows the collarbone (clavicle) and neck of a person from the front and a very important nerve that has three parts that dive through fascia above the collarbone. The second figure shows openings in the fascia to allow the nerve to make its way through more easily. These nerves or the fascia are very easy to damage since they are right on the surface. If the fascia does not work right it can “button hole” the nerve, as seen in the last figure. Because these nerves are so “claustrophobic,” they begin acting abnormally quickly.
The figure to the left below shows how sensory nerves travel along the skin and then suddenly dive through a layer of fascia to make their way between muscles to travel deeper toward the spinal cord. The first figure shows the collarbone (clavicle) and neck of a person from the front and a very important nerve that has three parts that dive through fascia above the collarbone. The second figure shows openings in the fascia to allow the nerve to make its way through more easily. These nerves or the fascia are very easy to damage since they are right on the surface. If the fascia does not work right it can “button hole” the nerve, as seen in the last figure. Because these nerves are so “claustrophobic,” they begin acting abnormally quickly.
|
Skin Nerves Are Easy to Keep Irritated by Muscle Contraction, Being Hit, or by Holding Positions; e.g., bad posture
Because muscles are contracting frequently, and because skin nerves are flat and often change direction suddenly to dive between muscle layers, the TRPV-1 nerves from the skin are easily irritated. Also, they are so easy to hit. For example, notice on this picture the location of nerves on the front of the knee. Hitting the knee cap or on the side of the knee cap could irritate these nerves and make them swell, and thus have more difficulty fitting through the hole in the fascia. |
How Can The Nerves Be Treated?
1. TOPICAL CREAM: Application of creams has been helpful in allowing patients to self-treatment of pain, particularly in nerves less severely affected. A recent clinical study has demonstrated that mannitol (a simple sugar alcohol) can decrease overactivity of the TRVP1 receptor. Thus far Vitamin D, dextrose, and mannitol have been observed to be helpful in creams applied on the skin. Formal clinical studies are in design or underway to confirm favorable effects seen in patients. These creams are best applied 2 times per day at a minimum. Examination of the whole nerve course is important because the nerves are not treated optimally by only placing the creams or solutions over the area of pain. Note that vitamin D and mannitol cream preparation for sale or distribution may be subject to patents not held by our office.
2. PERINEURAL INJECTION UNDER THE SKIN: It has been clinically observed that injection of dextrose (commonly with 5% dextrose) under the skin is analgesic to nerve pain, usually completely, and within seconds. This is consistent with a rapid block of that TRPV1 receptor as this occurs without anesthetic included. This typically needs to be repeated but after several treatments leads to progressive benefit, and according to ultrasound follow up shows evidence of stimulating healing of deeper structures. The first clinical study proving immediate analgesia from 5% dextrose without anesthetic was published in 2017. (See research tab)
3. PERINEURAL DEEP INJECTION: Injection about a nerve in a deeper region where it has to go around objects or through layers called “fascia” is also utilized, as it is at those points that nerve irritation can occur as well. This stretch by fluid, which had been recently found to be better done with dextrose than lidocaine alone, is called hydrodissection.
1. TOPICAL CREAM: Application of creams has been helpful in allowing patients to self-treatment of pain, particularly in nerves less severely affected. A recent clinical study has demonstrated that mannitol (a simple sugar alcohol) can decrease overactivity of the TRVP1 receptor. Thus far Vitamin D, dextrose, and mannitol have been observed to be helpful in creams applied on the skin. Formal clinical studies are in design or underway to confirm favorable effects seen in patients. These creams are best applied 2 times per day at a minimum. Examination of the whole nerve course is important because the nerves are not treated optimally by only placing the creams or solutions over the area of pain. Note that vitamin D and mannitol cream preparation for sale or distribution may be subject to patents not held by our office.
2. PERINEURAL INJECTION UNDER THE SKIN: It has been clinically observed that injection of dextrose (commonly with 5% dextrose) under the skin is analgesic to nerve pain, usually completely, and within seconds. This is consistent with a rapid block of that TRPV1 receptor as this occurs without anesthetic included. This typically needs to be repeated but after several treatments leads to progressive benefit, and according to ultrasound follow up shows evidence of stimulating healing of deeper structures. The first clinical study proving immediate analgesia from 5% dextrose without anesthetic was published in 2017. (See research tab)
3. PERINEURAL DEEP INJECTION: Injection about a nerve in a deeper region where it has to go around objects or through layers called “fascia” is also utilized, as it is at those points that nerve irritation can occur as well. This stretch by fluid, which had been recently found to be better done with dextrose than lidocaine alone, is called hydrodissection.