Karakilic GD, Aras PDM, Buyuk F, Bakirci ES. Prolotherapy Versus Phonophoresis and Corticosteroid Injections for the Treatment of Plantar Fasciitis: A Randomized, Double-Blind Clinical Trial. J Foot Ankle Surg. 2023. doi:10.1053/j.jfas.2023.04.010 Epub ahead of print. PMID: 37160200.
Here is a summary
•Design: Treatment comparisons study with randomized assignment of 18% dextrose DPT at 0, 2 and 4 weeks, steroid (40 mg methylprednisolone in anesthetic) injection at time 0. or 10 treatments of phonophoresis with 2% prednisolone gel for 20 minutes each session. Participants were advised to limit activity for 2 days after all procedures.
•Candidates: Heel pain > 3 months, pain with palpation at medial border of calcaneus, > 4 mm width of proximal plantar fascial, and unsuccessful conservative treatment.
•Study size: 146 patients were randomly divided but n's at points of follow-ups were not indicated to indicate if dropouts occurred.
•Bias: Randomized by drawing lots of equal numbers of papers with group type name written on them. (Not described well) It was not stated if baseline data was obtained prior to group assignment.
•Measures: Heel sensitivity index (HSI) 0-10 Pain scale, Foot Function Index, and Short Form 36. Plantar fascia thickness at 0, 1 and 3 months, unblinded.
•ITT versus Per Protocol: Not stated
•Other treatments: None
•Results: Groups were similar at baseline. All measure significantly decreased in all groups but no differences between groups except for heel sensitivity. That P value for heel sensitivity of .021 was likely not significant either. For multiple measures (four) the P value required for significance would be .05/4 or .013. (The correction of P values in studies with multiple measures in such a way, called a Bonferroni correction, is customary and usual)
Bottom line: This was a highly biased study in terms of limited description of allocation, randomization, and lack of mention of patient retention to the last follow-up point. The follow-up was short. No between group differences were seen taking into account the required P value correction for multiple groups. However, this was a large enough study to suggest that a meaningful benefit may occur from all 3 treatments for plantar fasciosis.
•Design: Treatment comparisons study with randomized assignment of 18% dextrose DPT at 0, 2 and 4 weeks, steroid (40 mg methylprednisolone in anesthetic) injection at time 0. or 10 treatments of phonophoresis with 2% prednisolone gel for 20 minutes each session. Participants were advised to limit activity for 2 days after all procedures.
•Candidates: Heel pain > 3 months, pain with palpation at medial border of calcaneus, > 4 mm width of proximal plantar fascial, and unsuccessful conservative treatment.
•Study size: 146 patients were randomly divided but n's at points of follow-ups were not indicated to indicate if dropouts occurred.
•Bias: Randomized by drawing lots of equal numbers of papers with group type name written on them. (Not described well) It was not stated if baseline data was obtained prior to group assignment.
•Measures: Heel sensitivity index (HSI) 0-10 Pain scale, Foot Function Index, and Short Form 36. Plantar fascia thickness at 0, 1 and 3 months, unblinded.
•ITT versus Per Protocol: Not stated
•Other treatments: None
•Results: Groups were similar at baseline. All measure significantly decreased in all groups but no differences between groups except for heel sensitivity. That P value for heel sensitivity of .021 was likely not significant either. For multiple measures (four) the P value required for significance would be .05/4 or .013. (The correction of P values in studies with multiple measures in such a way, called a Bonferroni correction, is customary and usual)
Bottom line: This was a highly biased study in terms of limited description of allocation, randomization, and lack of mention of patient retention to the last follow-up point. The follow-up was short. No between group differences were seen taking into account the required P value correction for multiple groups. However, this was a large enough study to suggest that a meaningful benefit may occur from all 3 treatments for plantar fasciosis.
Mansiz-Kaplan B, Nacir B, Pervane-Vural S, Duyur-Cakit B, Genc H. Effect of dextrose prolotherapy on pain intensity, disability, and plantar fascia thickness in unilateral plantar fasciitis: A randomized, controlled, double-blind study. Am J Phys Med Rehabil 2020;99:318-24.
Here is a summary
•Design: Double-blind, randomized, controlled study of injection of 15% dextrose (dextrose prolotherapy[DPT]) in .4% lidocaine twice at a three-week interval versus normal saline in .4% lidocaine at the same interval. Peppering technique with five needle contacts, “drilling the fascia.” Injection sites included metatarsal bone insertions, heel, and plantar fascia midpoint (not illustrated in the paper), with 1 ml at each location for a total of 5 ml injectate.
•Candidates: ≥ 6 months of pain and failure of conservative treatment for one month, plantar fascia thickness > 4 mm, and VAS pain > 5.
•Study size: 65 participants (32 DPT and 33 Saline)
•Bias: Computerized random number generation for group assignment by “a blinded clinician.”
•Measures: VAS pain (0-10), and the Functional Foot Index (FFI) to 15 weeks. Ultrasound measures at the same time of day. (9-10 AM)
•ITT versus Per Protocol: Per protocol. Three were lost from the saline group (2 of these were given dextrose injection open label due to severe pain) and two were lost from the dextrose group).
•Other treatments: Avoid heavy activities for three days after injection.
•Results: 1 in the control group and 2 in the DPT group had failed ESWT. Clinically significant improvements in both groups were reported, but DPT significantly outperformed saline injection for VAS and FFI. At 15 weeks the plantar fascia thickness decrease was significantly more in the DPT group, with a thickness less than 4 mm in 80% of DPT and 13.3% of saline groups and VAS score of 0 in 60% of DPT and 0% of saline participants.
Limitations: Short term study only to 15 weeks. Method not well described
Bottom Line 2020 Mansiz-Kaplan: Every 3 week DPT injection in multiple sites for plantar fasciosis outperforms normal saline injection @ 15 weeks
•Design: Double-blind, randomized, controlled study of injection of 15% dextrose (dextrose prolotherapy[DPT]) in .4% lidocaine twice at a three-week interval versus normal saline in .4% lidocaine at the same interval. Peppering technique with five needle contacts, “drilling the fascia.” Injection sites included metatarsal bone insertions, heel, and plantar fascia midpoint (not illustrated in the paper), with 1 ml at each location for a total of 5 ml injectate.
•Candidates: ≥ 6 months of pain and failure of conservative treatment for one month, plantar fascia thickness > 4 mm, and VAS pain > 5.
•Study size: 65 participants (32 DPT and 33 Saline)
•Bias: Computerized random number generation for group assignment by “a blinded clinician.”
•Measures: VAS pain (0-10), and the Functional Foot Index (FFI) to 15 weeks. Ultrasound measures at the same time of day. (9-10 AM)
•ITT versus Per Protocol: Per protocol. Three were lost from the saline group (2 of these were given dextrose injection open label due to severe pain) and two were lost from the dextrose group).
•Other treatments: Avoid heavy activities for three days after injection.
•Results: 1 in the control group and 2 in the DPT group had failed ESWT. Clinically significant improvements in both groups were reported, but DPT significantly outperformed saline injection for VAS and FFI. At 15 weeks the plantar fascia thickness decrease was significantly more in the DPT group, with a thickness less than 4 mm in 80% of DPT and 13.3% of saline groups and VAS score of 0 in 60% of DPT and 0% of saline participants.
Limitations: Short term study only to 15 weeks. Method not well described
Bottom Line 2020 Mansiz-Kaplan: Every 3 week DPT injection in multiple sites for plantar fasciosis outperforms normal saline injection @ 15 weeks
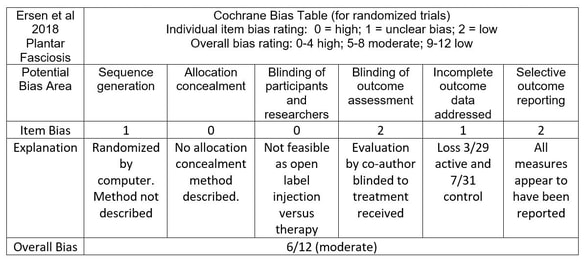
Ersen O, Akpancar S, Seven MM, Akyildiz F, Yildiz Y, Ozkan H. A randomized-controlled trial of prolotherapy injections in the treatment of plantar fasciitis. Turk J Phys Med Rehab 2018;64:59-65.
Here is a link to the full PDF of that article
Here is a link to the full PDF of that article
•Design: Randomized controlled study of 3 sessions at 3-week intervals of ultrasound-guided injection of 13.5% dextrose in .2% lidocaine into up to 5 different points versus plantar fascia and Achilles tendon stretching exercise three times weekly for three months under a therapist’s initial and intermittent guidance for 3 months and then instruction to perform exercises three times a day.
•Candidates: The duration and severity of symptoms was not stated. Those with a heel spur were excluded without a clear explanation as to why.
•Study size: 60 enrolled (DPT 29 and control 31)
•Allocation/Randomization Bias: Computerized assignment into two groups but it was not mentioned whether baseline data was obtained prior to revealing which group they were in. (Allocation was not described). Moderate bias for that reason.
•Measures: Visual Analog Scale (VAS), Foot and Ankle Outcome Score (FAOS), and Foot Function Index (FFI) at baseline and 1 year follow-up at last data collection. Excellent measurement tools.
•ITT versus Per Protocol: Per protocol (only 50 completed 1 years; 3 in DPT and 7 in control group were lost to follow-up)
•Other treatments: All participants were given heel lifts and instructed to refrain from heavy loading activities.
•Results: DPT outperformed saline on VAS and FAOS scores at 3 and 13 months. THE FFI was significantly better at three months but did not reach significance at 1 year, although the dextrose group trended. At one year 77% in the DPT group had more than 50% improvement in pain, compared to 17% in the control exercise group.
•Limitations: Candidates not clearly described. This would be level B- study evidence due to open label design and lack of adequate description of randomizaton and allocation.
•Bottom Line 2018 Ersen: Dextrose prolotherapy sessions every 3 weeks X 3 outperformed standard stretching exercises at 3 and 12 months
•Candidates: The duration and severity of symptoms was not stated. Those with a heel spur were excluded without a clear explanation as to why.
•Study size: 60 enrolled (DPT 29 and control 31)
•Allocation/Randomization Bias: Computerized assignment into two groups but it was not mentioned whether baseline data was obtained prior to revealing which group they were in. (Allocation was not described). Moderate bias for that reason.
•Measures: Visual Analog Scale (VAS), Foot and Ankle Outcome Score (FAOS), and Foot Function Index (FFI) at baseline and 1 year follow-up at last data collection. Excellent measurement tools.
•ITT versus Per Protocol: Per protocol (only 50 completed 1 years; 3 in DPT and 7 in control group were lost to follow-up)
•Other treatments: All participants were given heel lifts and instructed to refrain from heavy loading activities.
•Results: DPT outperformed saline on VAS and FAOS scores at 3 and 13 months. THE FFI was significantly better at three months but did not reach significance at 1 year, although the dextrose group trended. At one year 77% in the DPT group had more than 50% improvement in pain, compared to 17% in the control exercise group.
•Limitations: Candidates not clearly described. This would be level B- study evidence due to open label design and lack of adequate description of randomizaton and allocation.
•Bottom Line 2018 Ersen: Dextrose prolotherapy sessions every 3 weeks X 3 outperformed standard stretching exercises at 3 and 12 months
Risk of bias using Cochrane bias analysis
Atlas EU, Askin A, Tosun A. Is hypertonic dextrose injection effective in the treatment of plantar fasciitis: A clinical randomized study. The medical bulletin 2018; 56(3):102-108
Here is a summary :
Design: Randomized single blind controlled study of 3 sessions at 3 week intervals of injection of either 3 ml 15% dextrose (not stated if lidocaine was included) or 3 ml normal saline into plantar fascia-bone insertion point with peppering technique.
Candidates: Unilateral symptoms of plantar fasciosis (PF) for at least 2 months with minimal pain of 4 and pain over the calcaneal tubercle.
Study size: 30 enrolled, 15 in dextrose and 15 in saline groups.
Bias: Computerized assignment into 2 groups but who allocated and who was blinded other than the patient was not stated
Measures: (VAS score), foot function index (FFI), and American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot scores at 3 months.
ITT versus Per Protocol: ITT equivalent. It was explicitly stated that there were no dropouts.
Other treatments: Asked to avoid heavy loading for 3 days. Exercises were initiated 72 hours following the initial injections and were demonstrated to the patients on their first sessions, including daily plantar fascial stretching, towel carrying using toes, rolling solid objects with the sole, dorsiflexion against resistance, resisted plantar flexion, inversion and eversion
Results: Marked improvements in VAS, FFI and AOFAS scores at 3 months. DPT outperformed saline injection significantly.
Limitations: Small study with short follow-up to 3 months.
•Bottom Line 2018 Atlas: Every 3 week dextrose prolotherapy into plantar fascia origin outperformed saline injection @ 3 month follow-up.
Design: Randomized single blind controlled study of 3 sessions at 3 week intervals of injection of either 3 ml 15% dextrose (not stated if lidocaine was included) or 3 ml normal saline into plantar fascia-bone insertion point with peppering technique.
Candidates: Unilateral symptoms of plantar fasciosis (PF) for at least 2 months with minimal pain of 4 and pain over the calcaneal tubercle.
Study size: 30 enrolled, 15 in dextrose and 15 in saline groups.
Bias: Computerized assignment into 2 groups but who allocated and who was blinded other than the patient was not stated
Measures: (VAS score), foot function index (FFI), and American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot scores at 3 months.
ITT versus Per Protocol: ITT equivalent. It was explicitly stated that there were no dropouts.
Other treatments: Asked to avoid heavy loading for 3 days. Exercises were initiated 72 hours following the initial injections and were demonstrated to the patients on their first sessions, including daily plantar fascial stretching, towel carrying using toes, rolling solid objects with the sole, dorsiflexion against resistance, resisted plantar flexion, inversion and eversion
Results: Marked improvements in VAS, FFI and AOFAS scores at 3 months. DPT outperformed saline injection significantly.
Limitations: Small study with short follow-up to 3 months.
•Bottom Line 2018 Atlas: Every 3 week dextrose prolotherapy into plantar fascia origin outperformed saline injection @ 3 month follow-up.
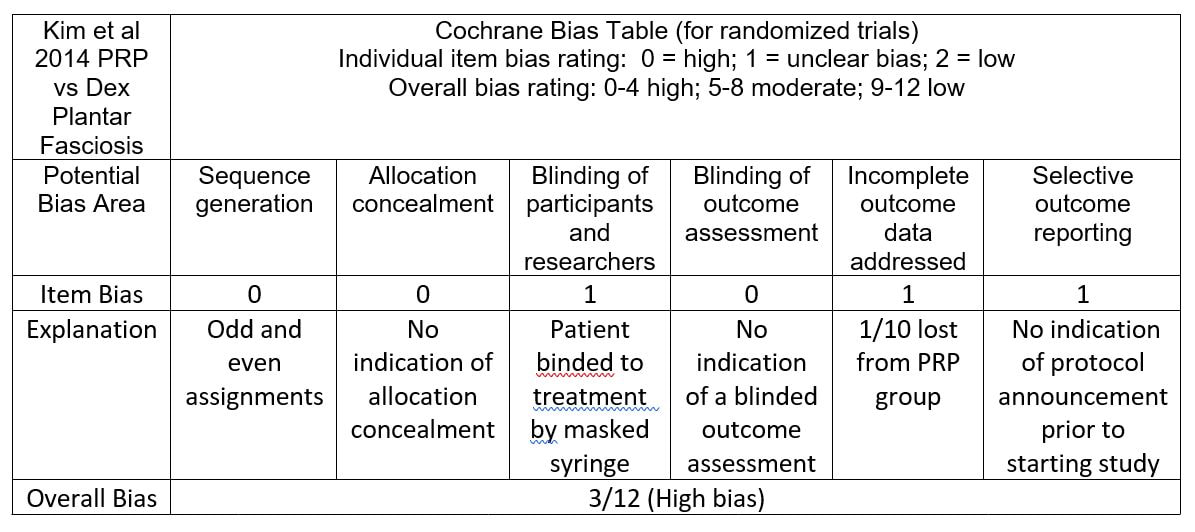
Kim E, Lee JH. Autologous platelet-rich plasma versus dextrose prolotherapy for the treatment of chronic recalcitrant plantar fasciitis. PMR 2014;6:152-8.
ABSTRACT
OBJECTIVE: To determine the efficacy of autologous platelet-rich plasma (PRP) compared with dextrose prolotherapy (DP) in patients with chronic recalcitrant plantar fasciitis (PF) DESIGN: A single-blinded, randomized, controlled study.
SETTING: Department of Physical Medicine and Rehabilitation of a university hospital.
PARTICIPANTS: Twenty-one patients with a clinical diagnosis of chronic PF confirmed by diagnostic ultrasound (plantar fascia thickness >4 mm) were randomly assigned to the PRP group (n = 10) or the DP group (n = 11).
INTERVENTIONS: Each patient received 2 injections into the plantar fascia through a peppering technique under ultrasound guidance at an interval of 2 weeks, either with 2 mL of autologous PRP or 2 mL of 15% dextrose/lidocaine solution.
MAIN OUTCOME MEASUREMENTS: The outcome measures included the pain, disability, and activity limitation subscales, measured by means of the Foot Functional Index. Data were collected before the first injection, at 2 weeks (before the second injection), and at the 2- and 6-month follow-ups.
RESULTS: All patients completed the follow-ups, with the exception of 1 patient in the PRP group. The mean Foot Functional Index total and subcategory score improvements were greater in the PRP group compared with the DP group (improvement with PRP vs DP, total: 30.4% vs 15.1%, pain: 29.7% vs 17.1%, disability: 26.6% vs 14.5%, activity limitation: 28.0% vs 12.4%). However, no statistically significant difference was noted at any follow-up. In the pain and disability subcategories, both groups showed significant improvements at the last re-evaluation. The PRP group also showed significant improvements in the disability and activity limitation subscales at the second re-evaluation.
CONCLUSIONS: Each treatment seems to be effective for chronic recalcitrant PF, expanding the treatment options for patients in whom conservative care has failed. PRP treatment also may lead to a better initial improvement in function compared with DP treatment.
SUMMARY Kim et al plantar fasciosis RCT
E. Kim et al. , using a method with high potential bias, compared dextrose prolotherapy to injection of autologous platelet rich plasma (PRP) in a 2-arm blinded trial. (Figure 35, table 6) Outcomes may have been affected by limited treatment to two times. Participants with chronic medial arch pain imitated with palpation over the plantar fascia origin and failure of conservative treatments such as NSAIDs, stretching PT, night split, arch supports or steroid injection) received injection at 0 and 2 weeks. Effects were assessed using the Foot Function Index (FFI). Data was collected before the first injection, and 2, 10 and 28 weeks after the last injection.
The two groups were statistically similar at baseline. The between-group difference in improvement on the FFI did not reach statistical significance at any point in time. (Figure 36) However, this is a comparison of two active treatment groups, both of which resulted in clinically significant improvement at more than twice the minimal perceptible change of 11.9 for the FFI in these participants with a mean pain duration of 2.9 years. This would be considered a positive treatmetn comparison study for dextrose prolotherapy, level of evidence B-.
E. Kim et al. , using a method with high potential bias, compared dextrose prolotherapy to injection of autologous platelet rich plasma (PRP) in a 2-arm blinded trial. (Figure 35, table 6) Outcomes may have been affected by limited treatment to two times. Participants with chronic medial arch pain imitated with palpation over the plantar fascia origin and failure of conservative treatments such as NSAIDs, stretching PT, night split, arch supports or steroid injection) received injection at 0 and 2 weeks. Effects were assessed using the Foot Function Index (FFI). Data was collected before the first injection, and 2, 10 and 28 weeks after the last injection.
The two groups were statistically similar at baseline. The between-group difference in improvement on the FFI did not reach statistical significance at any point in time. (Figure 36) However, this is a comparison of two active treatment groups, both of which resulted in clinically significant improvement at more than twice the minimal perceptible change of 11.9 for the FFI in these participants with a mean pain duration of 2.9 years. This would be considered a positive treatmetn comparison study for dextrose prolotherapy, level of evidence B-.